Fetal reduction is an important topic in modern medicine, especially in reproductive health. This procedure is significant for couples undergoing fertility treatments, such as in vitro fertilization (IVF), or those with high-risk pregnancies. It’s a complex decision with emotional, ethical, and medical layers. Understanding the basics of the procedure and the reasons behind it empowers you to make informed choices about your reproductive health.
What Is Fetal Reduction?
Fetal reduction involves reducing the number of fetuses in a multiple pregnancy. This step helps in promoting healthier pregnancies and outcomes when there are too many fetuses to safely carry to term. Several scenarios might necessitate this procedure, such as:
- Assisted reproductive technologies (ART) like IVF often lead to multiple pregnancies.
- Health concerns for any of the fetuses might warrant an embryo reduction procedure.
- High risks associated with carrying multiple fetuses for the mother’s health.
By opting for this, the likelihood of healthy babies increases, and potential complications can be minimized.
Medical Reasons for Fetal Reduction
There are sound medical reasons for considering fetal reduction. The procedure notably reduces the risks linked to multiple births. With fewer fetuses, there’s a decreased chance of complications like preterm births and health problems in newborns. For mothers, the benefits are clear in terms of reduced risk of pregnancy-induced conditions like hypertension or gestational diabetes.
The overall goal is to hopefully improve birth outcomes for mother and babies. With a more manageable number of pregnancies, health-related issues can often be navigated more effectively.
Timing and Procedure of Fetal Reduction
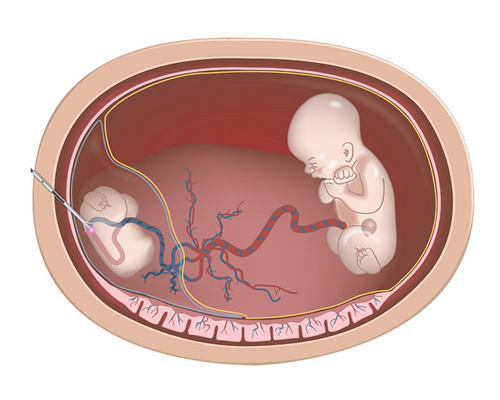
Fetal reduction is generally performed between 11 to 13 weeks of pregnancy. During this time, doctors use ultrasound guidance to perform the reduction. The procedure involves selecting the embryos to remove carefully while ensuring the remaining fetuses are nurtured optimally.
Here’s a simplified idea of the steps:
- Ultrasound Guidance: Ensures accuracy and safety.
- Selection Process: Focuses on the best outcome for the mother and infants.
- Procedure Execution: Conducted efficiently to ensure the least risk.
Risks and Benefits: Key Considerations
While fetal reduction carries risks, such as bleeding or miscarriage, these are rare. The benefits, however, often outweigh these risks. The procedure can significantly lower the chances of severe prematurity in infants. It also tends to improve maternal health outcomes. This balance of risks and benefits is why medical advice and emotional support are pivotal.
Navigating Emotional and Ethical Complexities
Fetal reduction is not just a medical decision but an emotional and ethical one. The procedure can have a profound emotional impact on parents. Feelings of loss, guilt, or relief may surface. Navigating these feelings requires counseling and psychological support.
Ethical considerations also arise. Each family’s circumstances vary, and what might be the best choice for one might not be for another. Compassionate counseling and support can help parents understand their feelings and align their decisions with their beliefs and values.
Decision-Making and Support
Before proceeding with fetal reduction, thorough discussion with healthcare providers and family is crucial. It’s important to have informed discussions and access multidisciplinary support. Maternal-fetal specialists provide necessary medical insights, while counseling services offer emotional support.
Here’s what to keep in mind while deciding:
- Discuss extensively: Talk with doctors and family to weigh all options.
- Seek support: Use available services like counseling and maternal-fetal advice.
- Be informed: Understand both the medical and emotional aspects involved.
After the Procedure: What to Expect
Recovery after fetal reduction involves both physical and emotional aspects. Physically, follow-up visits are crucial to monitor health and ensure recovery goes smoothly. Doctors will usually conduct check-ups to make sure everything is settling as expected.
Emotionally, recovery can be more complicated. Long-term support and counseling might be beneficial to process feelings fully. Speaking with professionals or support groups can help individuals find peace with their journey.
Advancements and Alternatives
With advancements in medical technology, fetal reduction has become safer and more effective. Technology aids decision-making by providing clearer insights and better procedural outcomes. There are also alternative options and lifestyle choices that expectant parents can explore.
Understanding these alternatives offers more control and aligns expectations with personal health goals. Engaging with developing technologies and seeking continual guidance can bring reassurance.
Conclusion: Embracing a Personal Journey
Fetal reduction is more than just a medical procedure. It’s a personal journey requiring careful thought and support. Making informed decisions and consulting specialists are vital steps.
Support is always available. Make use of resources when considering selective fetal reduction. Health providers and counselors offer assistance and guidance for those navigating this multifaceted process. Remember, every journey is unique, and making the best choice for your situation is what truly matters.